Hello, friends. This evening I’m writing to you from my office cozy with its string lights and Hershey’s cushions and blankets all over the floor, cocooned and insulated from the shivering depths of our desert valley. We’ve been having a spring cold spell with temps in the 60’s all week. Today the high was a teeth-chattering 66 degrees F, and yesterday the high was 64, which to me is a crazy Arctic blast.
I didn’t mean to be delinquent here last week! I wanted to post, but I found that I couldn’t make a decision, so I ended up walking away from my laptop.
I’ve been going back and forth trying to decide whether to keep you apprised of medical updates and such. I figure you’ve been along with me for the ride so you may want to know what’s going on, but I wasn’t sure how much I wanted this blog to be about my health – there’s been a lot of that lately. However, I did go to the pulmonologist last week, so I have updates. I finally decided to go ahead and share these and future updates with you. I promise there’ll be more to this blog than medical stuff, though!
First, a quick look at the current situation of my swelling in the aftermath of gum-graft surgery. It’s coming along! That area of my jaw is still tender to the touch on both sides, but the swelling is gradually going down, just as I was told it would. “Gradual” is right.

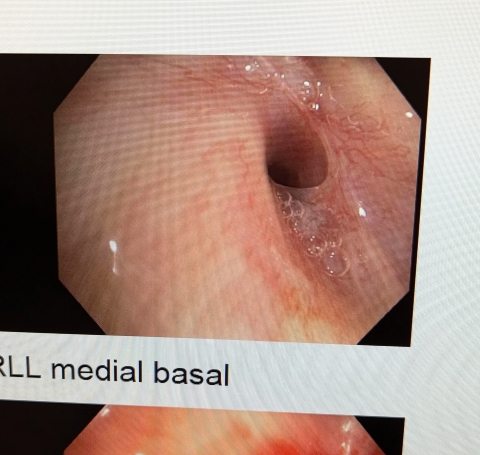
About Charlotte the Lung, then.
Charlotte’s latest CT scan (two weeks ago) looks worse than last year’s. My partial lung collapse (atelectasis) hasn’t changed, but “mild bronchiectasis” (April 2024) is now “traction bronchiectasis” likely due to fibrosis (scarring). The scan also shows “multifocal areas of endobronchial debris or mucous plugging,” which seems to be a product of Sjögren’s Syndrome. My pulmonologist believes that Sjögren’s is complicating matters for Charlotte.
My updated pulmonary function test shows changes for the worse in a couple of areas, as well.
Because of these results, I’m now on a different medication, and we’re going to repeat the CT scan and recheck my pulmonary function in six months. Doctor said that depending on those results, he might want to perform a second bronchoscopy, and also treat my lung infection. We’ve been taking a “wait and watch” approach to the infection, since it’s low-grade and the treatment is aggressive.
Despite these disappointing test results, I’m still incredibly grateful to have lungs that work, structural abnormalities aside. I can’t hike, swim, or sing the way I used to, but I can breathe. I don’t need oxygen!
Week after next I have an appointment with my neurologist, so that week’s post will include Agatha the Brain updates.
May this post find you doing well with your health and well-being, friends. Thank you so much for reading, for still being here. It means a lot.
Until next time!